The public sector is made up of organizations that are owned and operated by the government and provide services for the citizens in the U.S. Public sector programs can have a meaningful and significant influence on both individual and community health. Public sector programs and health policies are often put in place by the government to provide healthcare and services to individuals who are unable to afford it on their own (Longest, 2016).
Over the last 100 years the U.S. government has put in place policies and programs to promote maternal and infant health.

In 1921, Congress passed the Maternity and Infancy Act which allowed states to be funded with grants to develop health services for mothers and children (Longest, 2016). This was the first federally funded social welfare program and was intended to reduce the alarming rates of maternal and infant mortality. Using their newly won voting rights, women urged Congress to pass the 5-year program and renew it in 1926. However, with the Supreme Court question of its constitutionality and opposition from the American Medical Association, the act was terminated in 1929 (U.S. Capitol, n.d.).
In 1963, the Social Security Act of 1935 was amended with the Maternal and Child Health and Mental Retardation Planning Amendments with the goal of expanding and refining maternal and child health programs that would improve care for individuals with conditions associated with childbearing that may lead to mental retardation (Longest, 2016).

In 1965, Medicaid was enacted as a new title to the Social Security Act as a federal and state program to pay for medical assistance for individuals and families with low income and resources. Medicaid ensures medical assistance for certain basic services, allowing women to seek pregnancy related services, including prenatal care and 60 days postpartum pregnancy-related services, from physicians, nurse practitioners, and nurse-midwives (Longest, 2016).
In 1970, The Family Planning Services and Population Research Act, also known as the Title X Family Planning program, was passed with bipartisan approval. This was a significant advancement in women’s health in the public sector, because this act provided women resources to aid in family planning no matter their economic conditions. The Act provided funding to both public and nonprofit private organizations to develop comprehensive family planning programs and aimed to improve the administration of family planning services and population research programs. Most importantly, it made comprehensive family planning services, available to low income and uninsured families. It is the only federal grant program dedicated solely to providing comprehensive family planning and related preventive health services (Longest, 2016; Office of Population Affairs, 2019).

In 1972, the Child Nutrition Act was amended to establish the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) (Longest, 2016). This program provides federal grants to states for supplemental food, health care referrals, and information on healthy eating for low-income pregnant, breastfeeding, and non-breastfeeding postpartum women, and to infants and children up to age five who are found to be at nutritional risk. Studies have proven WIC to be one of the nation’s most successful and cost-effective nutrition intervention programs. It has led to a greater likelihood of receiving prenatal care, longer pregnancies, higher maternal hemoglobin levels and lower risk of maternal obesity in subsequent pregnancies, fewer premature births, low incidence of low birth weight babies, fewer incidents of infant death, and a health care cost savings of $1.77 to $3.13 on every dollar spent on the program (U.S. Department of Agriculture, n.d.).
In 1977, the Rural Health Clinic Services Amendments was put in place to allow reimbursement of services provided by nurse practitioners and physician assistants to Medicaid beneficiaries seeking care in clinics in rural settings (Longest, 2016). This act is extremely important to maternal health since women who live in rural areas are at higher risk for maternal morbidity and mortality.
In 1986, Congress enacted the Emergency Medical Treatment and Active Labor (EMTALA) to ensure hospitals treat and stabilize patients regardless of their ability to pay, including women in labor (Longest, 2016).
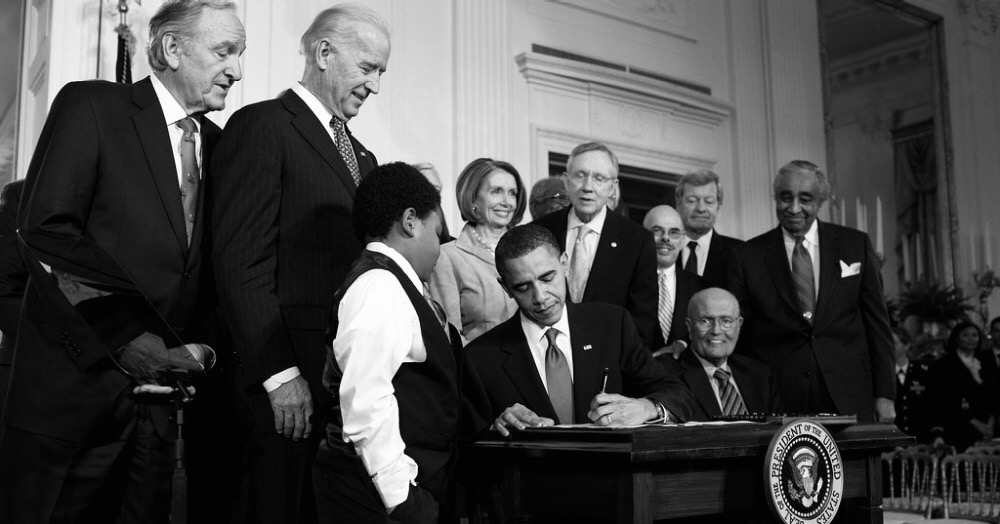
In 2010, the Patient Protection and Affordable Care Act was passed into law. This major health reform law increased access to affordable health insurance for the millions of Americans without coverage, made health insurance more affordable for those who already had it, and expanded Medicaid eligibility (Longest, 2016), increasing access to healthcare for millions of women.

Current Public Sector Programs and Initiatives Focused on Maternal and Women’s Health
Alliance for Innovation on Maternal Health (AIM) Maternal Health and Safety Initiative: AIM assists with the implementation of maternal safety bundles to improve the quality and safety of maternity care to reduce maternal morbidity and mortality. These safety bundles are straightforward sets of evidence-based practices that have been shown to improve patient outcomes. The AIM safety bundles include:
- Obstetric Hemorrhage
- Severe Hypertension in Pregnancy
- Maternal Venous Thromboembolism Prevention
- Safe Reduction of Primary Cesarean Birth
- Supporting Intended Vaginal Births
- Reduction of Peripartum Racial/Ethnic Disparities
- Postpartum Care Basics for Maternal Safety from Birth to the Comprehensive Postpartum Visit
- Postpartum Care Basics for Maternal Safety Transition from Maternity to Well-Woman Care
- Obstetric Care for Women with Opioid Use Disorder
Women’s Preventive Service Initiative: 5-year effort that aims to improve women’s health across the lifespan and access to high-quality health care through preventive services, including screening for gestational diabetes, breastfeeding support, supplies, and counseling, screening for diabetes after pregnancy, and contraceptive methods and counseling.
Healthy Start: Eliminating Racial/Ethnic Disparities: This program has a goal to reduce the rate of infant mortality, improve perinatal health, and reduce racial and ethnic disparities in high-risk communities through community-based approaches to service delivery and increase access to comprehensive health and social services for women and their families.
The Maternal, Infant, and Early Childhood Home Visiting Program: This program provides home visitation by trained professionals to at-risk expectant parents or families with young children. They provide services to build strong, healthy families through teaching positive parenting skills and parent-child interactions, promoting early learning and communication, guidance on breastfeeding, safe sleep, injury prevention, and nutrition, screening of postpartum depression, substance abuse, and domestic violence, and providing adequate family resources.
(Health Resources and Services Administration, Maternal and Child Health, 2020).
Public sector programs and policies are vital to improving the well-being of mothers and their families. Ensuring the well-being of women determines the health of the following generations and can help prevent future public health challenges for families, communities, and the healthcare system as a whole.
References
Health Resources and Services Administration, Maternal and Child Health. (2020). Programs and initiatives. Retrieved from https://mchb.hrsa.gov/maternal-child-health-initiatives/mchb-programs
Longest, B. B., Jr. (2016). Health policymaking in the United States. Chicago, IL: Health Administration Press.
U.S. Capitol Visitor Center. (n.d.). Protecting mothers and infants. Retrieved from https://www.visitthecapitol.gov/exhibitions/april-2010-september-2011/protecting-mothers-and-infants
U.S. Department of Agriculture, Food and Nutrition Services. (n.d.). Special Supplemental Nutrition Program for Women, Infants, and Children (WIC). Retrieved from https://www.fns.usda.gov/wic
U.S. Department of Health and Human Services, Office of Population Affairs. (2019). Title X Family Planning. Retrieved from https://www.hhs.gov/opa/title-x-family-planning/index.html
Hi Kara-
It is wonderful to see how many services there are for pregnant and postpartum women. Public sector support is crucial in providing women and children with the resources they need to remain healthy. While there is great support, there is still room for improvement. One major concern that many have regarding Medicaid for low income pregnant women is the period of time for which the services are offered. Pregnancy related coverage only extends for 60 days after birth for the mother and one year after birth for the infant. Women who are low income, and thus likely utilizing Medicaid, are more likely to have chronic conditions and risk factors that lead to negative maternal health and birth outcomes (MacPac, 2018). Among pregnancy related deaths, 11.7% occurred 43-365 days postpartum, with the most common causes being infection, cardiomyopathy, and pulmonary embolism (Peterson et al., 2019). Sixty percent of those deaths were deemed to have been preventable. Contributing factors to women not seeking the medical attention they needed during this time frame included gaps in insurance coverage, lack of access to clinical care, and lack of transportation to medical facility. Extending Medicaid coverage to 365 days postpartum would address each of these points and provide these mothers with the preventative services they need.
References
Medicaid and CHIP Payment and Access Commission. (2018). Pregnant women and Medicaid. Retrieved from: https://www.macpac.gov/wp-content/uploads/2018/11/Pregnant-Women-and-Medicaid.pdf
Peterson, E., Davis, N., Goodman, D., Cox, S., Mayes, N., Johnston, E….. & Barfield, W. (2019). Vital signs: Pregnancy related deaths, United States, 2011-2015, and strategies for prevention, 13 states, 2013-2017. Centers for Disease Control and Prevention, 68(18), 423-429. Retrieved from: https://www.cdc.gov/mmwr/volumes/68/wr/mm6818e1.htm?s_cid=mm6818e1_w#T2_down
LikeLike
I enjoyed reading about the progress we have made over the years in maternal health within the public sector. I did some research on the Ailliance for for Innovation on Maternal Health (AIM) because I was curious why Arizona had not yet joined this alliance. I found that although we are not currently enrolled, we have begun the process of becoming enrolled in AIM. In October of 2018, the Severe Maternal Morbidity/Maternal Mortality Prevention Taskforce was created in Arizona (Cunningham, 2019). This task force has been meeting since then to discuss ways to improve maternal health in our state. One of the topics of discussion at multiple meetings has been becoming a member of the AIM (Cunningham, 2019). The taskforce works along with March of Dimes and the Arizona Perinatal Trust to determine which issues are prevalent in maternal health and strategies to work on these issues within the realm of public policy (Cunningham, 2019). The issues they have focused on include acute problems like hemorrhage and hypertensive emergencies, as well as social determinants of health such as access to care and income level (Cunningham, 2019). I am hopeful that this taskforce will accomplish a great deal of work in the coming years to help decrease our high rates of maternal mortality.
Here is a link to the meeting agendas for past meetings of the taskforce: https://azdhs.gov/prevention/womens-childrens-health/index.php#mmm-az-meetings-task-force
References:
Cunningham, M.E. (2019, Sept 16). Arizona’s efforts to reduce maternal mortality and severe maternal morbidity [Blog Post]. Retrieved from http://www.azpha.org/wills-blog/category/Maternal+Health
LikeLike
Your blog was very insightful on public sector programs to reduce maternal and infant mortality. I was especially intrigued by the Maternal, Infant, and Early Childhood Home Visiting Program.
I had never heard of this program before but after reading about it on your blog I had to visit their website to learn more information.
Did you know that their program is evidence-based? The home visiting program could benefit so many at risk women, infants, and families. In 2019, the program improved maternal and newborn health, school readiness and achievement, and family economic self-sufficiency (Health Resources & Service Administration, Maternal & Child Health, 2020). As a healthcare provider it is so important to know that these services exist and to be educated on them so we can encourage eligible patients to use them. Thanks for sharing!
References
Health Resources & Service Administration, Maternal & Child Health. (2020). Home visiting. Retrieved from https://mchb.hrsa.gov/maternal-child-health-initiatives/home-visiting-overview
LikeLike
Kara,
Thank you for your informative blog. The issue of maternal morbidity and mortality is a long-standing issue. One would expect that with advancements in healthcare technology that this issue would be decreasing. However, in addition to health disparities, women are getting and staying pregnant today with chronic conditions that would have not been possible just a decade ago.
Perinatal and postpartum infections that develop into sepsis. These infections are often a significant cause of maternal morbidity and mortality (Phillips & Walsh, 2020; Society for Maternal Fetal Medicine [SMFM], Plante, Pacheco, & Louis, 2019). At my current workplace, I have seen an increase in readmissions for infections. These women often have a chronic condition that places them at risk for an infection. Infections are the result of often-treatable conditions that contribute to a high rate of morbidity and mortality when they are not recognized and treated promptly. Risk factors include nulliparity, black race, public or no insurance, and low socioeconomic status. Increasing awareness of risk factors that are exacerbated through health disparities and low health literacy can help increase system-level and health policy improvements that will improve long term outcomes. Increasing provider knowledge of risk factors and signs and symptoms of worsening maternal conditions will allow for prompt intervention.
Thank you for addressing this important topic. It needs increased awareness within the healthcare community as well as with policymakers to improve outcomes in this country.
Brittany
References
Phillips, C. & Walsh, E. (2020). Group A streptococcal infection during pregnancy and the postpartum period. Nursing for Women’s Health. 24 (1), 13-23. Doi: 10.1016/j.nwh.2019.11.006
Society for Maternal Fetal Medicine, Plante, L. A., Pacheco, L. D., & Luis, J. M. (2019). SMFM consult series #47: Sepsis during pregnancy and the puerperium. American Journal of Obstetrics & Gynecology. 220 (4), B2-B10. Doi: 10.1016/j.ajog.2019.01.216
LikeLike
Kara,
I really found your blog to be very interesting and informative. I as not aware of all the public sector initiatives that had been supported about maternal health over the past century. The only program I had heard of prior to reading your blog was the Women Infants & Children (WIC) program.
It is very interesting to read about the 1921, Sheppard-Towner Maternity and Infancy Act. This act that provided $1 million per year for a five-year period to help the states combat the high infant and mother mortality rates (“Maternity and Infancy Act,” n.d.). This act is credited with being one of the landmarks in the creation of social welfare programs in the U.S. (“Maternity and Infancy Act,” n.d.). We now know that these programs were history making and monumental reforms that have helped millions of Americans over the last century. It does seem that we have come a long way from new voting rights for women to the Sheppard-Towner Act of 1921 to the Affordable Care Act of 2008. We can still make improvements to public sector policy and how we implement those policies. Learning that it has taken a century to get that far gives perspective on just how things work with and function in the public sector. It was designed to move slowly in such a way that one person or group could not make too much change too quickly, without the consent of the entirety of this society.
References:
The Sheppard–Towner Maternity and Infancy Act. (n.d.). Retrieved from https://history.house.gov/Historical-Highlights/1901-1950/The-Sheppard%E2%80%93Towner-Maternity-and-Infancy-Act/
LikeLike