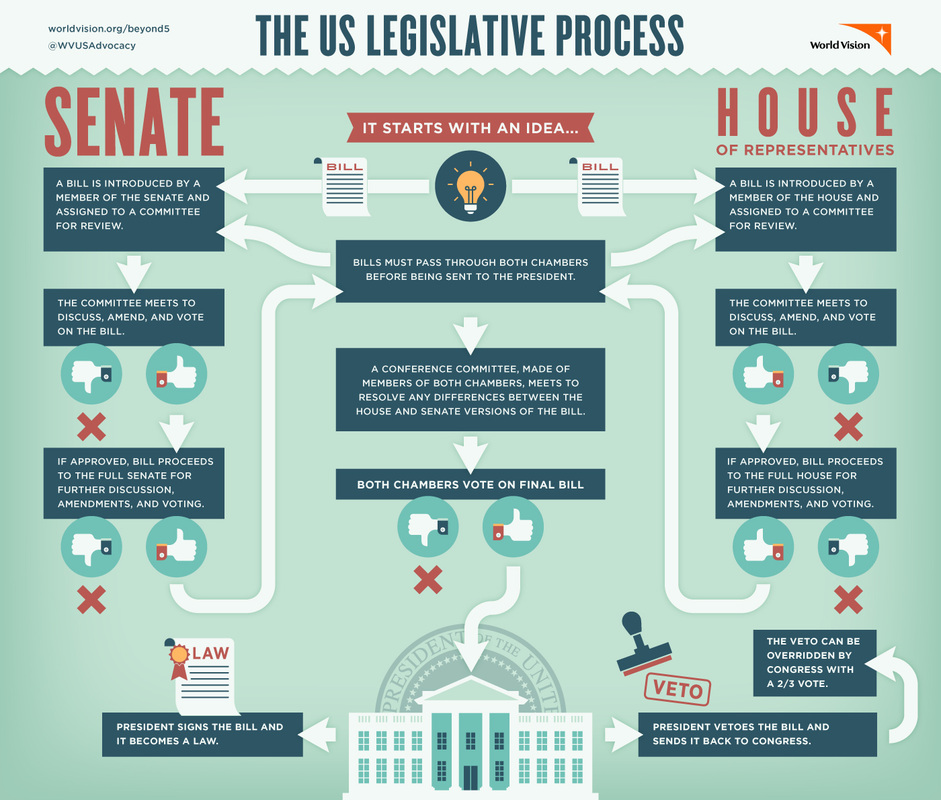
In order to understand current legislation addressing maternal mortality, we first need to understand the process of bills becoming laws. Anyone can come up with an idea for a bill, such as constituents (the voting public), a member of Congress, the president or the Executive Branch (Longest, 2016). However, only a member of either the House of Representatives or the Senate can introduce a bill. Based on the subject matter of a bill it will be assigned to a committee to review, amend, and vote on a bill. If a bill passes through a committee, it then moves to the floor for consideration, possible amending, and a vote. Both the House of Representatives and the Senate must pass a bill before it is sent to the president to sign the bill into law (The United States House of Representatives, n.d.). The process of a bill becoming a law is cumbersome, but this prevents the passing of senseless or dangerous laws. Understanding the complex judicial system and the law-making process can be tedious; the graphic below illustrates the progression.
The Institutions and Actors
Individuals, organizations, and interest groups all contribute to the development of legislation. Interest groups are particularly influential due to their resources. Legislators are often motivated to amend or repeal existing laws or introduce new laws based upon the problems that directly affect their constituents or society as a whole. The members of Congress serve the important role of sponsoring or endorsing bills to move them into committee review. The legislative committees and subcommittees within both House of Representatives and Senate operate as essential institutions for moving proposed ideas through the legislative process. The president arguably has the most control with the ability to veto a bill (Longest, 2016).
Statutory and Regulatory Mechanisms
So now that we understand the process of bills, we can evaluate what has been done and what is currently in process in terms of maternal mortality. Legislation regarding maternal mortality and its contributing factors is relatively new.
2016: H.R.34- 21st Century Cures Act. Bringing Postpartum Depression Out of the Shadows Act
A part of this Act addressed the use of federal grant money to develop and/or maintain maternal mental health programs to educate, screen, and treat postpartum depression (March for Moms, 2019).
2018: H.R.315/S.783- Improving Access to Maternity Care Act
This Act addresses the maternity health care provider shortage and helps identify the areas of greatest need (March for Moms, 2019).
2018: H.R.1318/S.1112- Preventing Maternal Deaths Act
This was the Act discussed in my first blog post. This bipartisan bill establishes a program under the Department of Health and Human Services which provides grants for states to establish and support committees to review every maternal death and based on those findings develop recommendations on how to prevent future deaths (March for Moms, 2019).
Active Legislation
H.R.4995 The Maternal Health Quality Improvement Act
This bill establishes grants for rural obstetric networks to improve access to care, telehealth resources for maternal care providers, training for providers practicing in rural areas, training for providers in implicit and explicit bias, and integrated services for pregnant and postpartum women (March for Moms, 2019).
H.R.4996 The Helping Medicaid Offer Maternity Care Services (MOMS) Act
This bill gives states the option to extend Medicaid and Children’s Health Insurance Program (CHIP) coverage from 60 days to one year postpartum for women who have pregnancy-related Medicaid or CHIP coverage. It will increase the state’s federal matching rate of 5% for one year. It also addresses Medicaid policies for the reimbursement of doula services (March for Moms, 2019).
What can you do?

Contact your legislator and voice your support of these active bills that directly benefit mothers in the United States. People that schedule meetings and directly speak to their legislator generally have their voices heard and increase their influence. Mobilizing support, writing letters, sending delegations, and motivating allies to join efforts can get the attention of government officials (Kingdon, 2011). As discussed above, the legislative process has many steps. The more support a bill garners, the easier the progression of it will be.
References
Kingdon, J.W. (2010). Agendas, Alternatives, and Public Policies, Updated Second Edition. London: Longman Publishing Group
Longest, B. B., Jr. (2016). Health policymaking in the United States. Chicago, IL: Health Administration Press.
March for Moms. (2019). Federal legislation. Retrieved from https://marchformoms.org/advocacy/federal-legislation/
The United States House of Representatives. (n.d). The legislative process. Retrieved from https://www.house.gov/the-house-explained/the-legislative-process
This post comes at an opportune time for me, as I just recently had the privilege of participating in the March of Dimes public policy day at the Arizona Capitol. Along with other constituents from my legislative district, I met with my representatives to discuss several bills related to maternal and newborn care. The ones that most directly relate to your blog post were:
S. 1290: This bill would establish a Maternal Mental Health Advisory Committee with the purpose of recommending improvements for screening and treating perinatal mood and anxiety disorders. These recommendations would be brought to the legislature in a report by the end of 2021 (S. 1290, 2020).
S. 1392: This bill seeks to extend coverage for women up to a year postpartum. Currently, if patients fall below 161% of the federal poverty line, they have coverage for up to 56 days postpartum. Women who fall below 138% of the federal poverty line can then receive insurance through other government programs, but this means that women between 138% and 161% (about 3,000 women annually), lose their health insurance entirely (S. 1392, 2020).
These two bills would have a huge impact on women in our state. The year following the birth of a child is a time when women are at high risk for health issues, including psychiatric conditions related to perinatal mood disorders, cardiovascular complications such as stroke and heart attack, and complications related to diabetes (American College of Obstetricians and Gynecologists [ACOG], 2018). In addition, they are navigating all of the obstacles that come with having a new baby to take care of. It is so important as healthcare providers to advocate for the proper care for women during this sensitive time in their lives.
References:
American College of Obstetricians and Gynecologists (ACOG). (2018). Optimizing postpartum care. Obstetrics & Gynecology, 131(5), e140-e150.
S. 1290, 54th Legislature. (2020).
S. 1392, 54th Legislature. (2020).
LikeLike
Who are the nongovernmental actors engaged in advocacy around the current pending legislation?
LikeLike